INTRODUCTION
Schizophrenia is one of the most disabling medical disorder. Considered a severe mental illness (SMI), it is usually associated with impaired social and occupational functioning. Approximately seven people per 1,000 will experience it in their lifetime (McGrath et al., 2008). The economic burden of schizophrenia diagnosis and treatment was estimated at $155.7 billion USD in 2013 in the United States (US) (Cloutier et al., 2016), including health costs and those associated with productivity loss. Indeed, the mortality rate of people with schizophrenia more than doubles that of the general population, largely due to the high prevalence of comorbid physical conditions (McGrath et al., 2008), which may be associated with their limited healthcare access.
Patients with schizophrenia have a shorter life expectancy (Laursen et al., 2014) due to poor physical health, which may be associated with worse health habits (such as substance use). There may also be barriers to the adequate physical care of this population, associated with both the patient and their illness, and compounded by the attitudes of physicians and the healthcare organizational structure (McGinty et al., 2015). A fragmented healthcare system, limited healthcare access, the inability of these patients to identify their medical problems or reluctance to be treated may contribute to their poor physical healthcare (Lambert et al., 2003). The frequent stigmatization of psychiatric patients (even among physicians) may exacerbate the problem (Copeland et al., 2006; Leucht et al., 2007).
In the initial reviews of this research issue, Goldman (1999) found that 50% of patients with schizophrenia had a comorbid or undiagnosed medical pathology. These patients were often excluded from research studies (Jeste et al., 1996), making it difficult to determine the extent and consequences of this healthcare deficit. Lambert et al. (2003) noted that patients with schizophrenia had a life expectancy ten to 25 years lower than that of the general population, while other authors have observed that this difference can increase over time (Hjorthøj et al., 2017; Laursen et al., 2014; Leucht et al., 2007). Lee et al. (2018) reviewed eight longitudinal studies of mortality in schizophrenia, finding that the standardized mortality rate (SMR) of these patients compared to that of the general population increased by 37% from 2.2 in pre-1970s studies to 3.0 in post-1970s reports.
Salokangas (2007) reviewed studies of patients with schizophrenia living in community residences, observing that most had undetected physical illnesses, despite seeking medical care more frequently than the general population. The literature review by Leucht et al. (2007) found a higher prevalence of human immunodeficiency virus (HIV) infection and hepatitis, osteoporosis, altered pain sensitivity, sexual dysfunction, obstetric complications, cardiovascular diseases, overweight, diabetes, dental problems, and polydipsia than among the general population. Likewise, Oud and Meyboom-de Jong (2009) systematically reviewed the prevalence and treatment of somatic comorbidity in primary care, finding that patients with serious mental illness (SMI) were at risk of developing diabetes mellitus, metabolic syndrome, hypertension, cardiovascular or pulmonary diseases, hypothyroidism, and visual problems. A number of reviews conducted in this century have identified a group of physical health issues commonly found in individuals with SMI. These comorbidities include, but are not limited to, diabetes, and cardiovascular, infectious, metabolic, and hormonal diseases. Most of these health concerns are associated with genetic and lifestyle factors, and are compounded by the inability of these patients to identify their medical problems, reluctance to be treated or their inadequate medical assessment. Consequently, these characteristics have become a typical pattern in the lives of most individuals with schizophrenia, negatively impacting their quality of life, life expectancy, and healthcare. To the authors’ knowledge, there is a dearth of systematic medical literature reviews exploring the impact of somatic comorbidity on patients with schizophrenia. In addition, according to the most recent reviews, the severity of this mental disorder is due to its increasing mortality, pointing to a possible relationship between this psychiatric diagnosis and severe physical diseases such as cancer, diabetes mellitus, and certain chronic cardiovascular diseases (Laursen et al., 2014; Nordentoft et al., 2021; Rodrigues et al., 2021). For instance, Nordentoft et al. (2021) found that patients with schizophrenia have a 50% higher risk of breast, lung, and colon cancer deaths than the general population, while Nordentoft et al. (2021) observed that those with psychotic disorders have a 69% higher risk of multimorbidity (the occurrence of multiple co-occurring, chronic conditions in which the chronic cardiovascular disease may be hypertension, coronary heart disease, myocardial infarction, ischemic stroke, or atrial fibrillation).
Kowalski and Misiak (2023) recently reviewed the multidimensional associations between schizophrenia and COVID-19 for common biological pathways, finding that environmental stress, common comorbidities of schizophrenia, and the adverse effects of antipsychotic treatment are associated with greater severity and mortality of the disease. The present systematic review aims to examine the physical comorbidity of patients diagnosed with schizophrenia, regardless of the level of severity, and the healthcare received. It also specifically seeks to determine how this relationship impacts the mortality of these SMI patients, identify the main physical conditions comorbid with a diagnosis of schizophrenia; and observe the healthcare service utilization of these patients with comorbid physical conditions to gauge the degree of access to and quality of the medical treatment they receive, and the hospital admissions rate.
METHOD
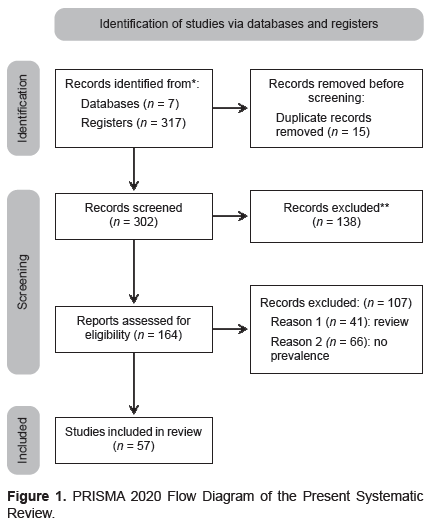
The systematic review protocol has been registered with the PROSPERO database (registration number: CRD42020139972) and adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009; Urrútia, & Bonfill, 2010; Page et al., 2021).
Inclusion and exclusion criteria
To be eligible for consideration, research studies must be original observations published in reputable, peer-reviewed journals and include cross-sectional studies of cohorts, cases and controls. Cohort studies are included in the present study because they typically involve analytical and observational research requiring at least one group of patients diagnosed with this SMI. The main methodological objective is to identify the relationship between risk factors, such as physical comorbidities, and health outcomes such as morbidity and mortality. Case-control studies are another type of observational research commonly used in healthcare settings to establish potential links between psychiatric disorders and physical comorbidities. They may also be experimental designs comparing these SMI patients with the general population, providing valuable insights. This latter type of study analyzes variations between patients with a diagnosis of schizophrenia and those without psychiatric conditions in regard to mortality, physical comorbidity, such as the occurrence of physical diseases, clinical traits of physical illnesses, prognosis, and healthcare service utilization (including length of stay, outpatient appointments, emergency room visits, and expenses).
The methodological decisions determining the selection of empirical papers sought to include the research associated with the aims of this study. Only publications in English, Spanish, and French were included, since these are the languages in which the authors are proficient.
To ensure accuracy, we excluded clinical cases, case series, and case studies with only one subject (N = 1). We also eliminated reviews, meta-analyses, theoretical studies, and clinical trials. No restrictions were placed on the healthcare environment or type of treatment, and the date of publication was unimportant.
Search strategy
We performed an extensive search of the literature in 2021 in scientific databases such as PubMed/MEDLINE, EMBASE, Scopus, Web of Science, PsycINFO, Cochrane Library, and ProQuest Health Research Premium Collection to collect relevant information (see Figure 1 for further details; Page et al., 2021). The search was narrowed down from 1/1/1991 to 31/12/2021.
To find the information, a search strategy was implemented involving a combination of specific terms such as “Schizophrenia” [Mesh] AND “Comorbidity” [Mesh], “Schizophrenia” [Title] AND (“medical comorbidity” OR “physical comorbidity”). We also examined the studies found in the search for any relevant references.
Selection of studies and data extraction
Two authors conducted a review of the titles and abstracts of the studies retrieved to identify potential studies that met the inclusion criteria. In addition, they manually scrutinized the reference lists of eligible publications. The two reviewers independently evaluated the full text of potentially eligible studies. They resolved discrepancies through deliberation, consulting with the last author when necessary. Thereafter, the first author meticulously analyzed each paper selected to prepare a first draft of the results summarized in the tables, which were subsequently reviewed by the third author. This involved scrutinizing the Method section to check the research design, and conduct a detailed analysis of the title, abstract, introduction (objectives), method, and results sections to extract the critical variables of the study listed in Tables 1 and 2, which include the author, design, country, year of publication, study design, sample size, age range of the sample, sex distribution, results, measures, and main conclusions.
RESULTS
A meticulous search of seven scientific databases yielded 317 entries. Removing the duplicates left 302 entries. The elimination of 138 irrelevant articles narrowed the focus to 164 relevant items. Finally, after conducting a thorough analysis of each full-text article, we identified 57 publications that met our stringent inclusion criteria (Figure 1).
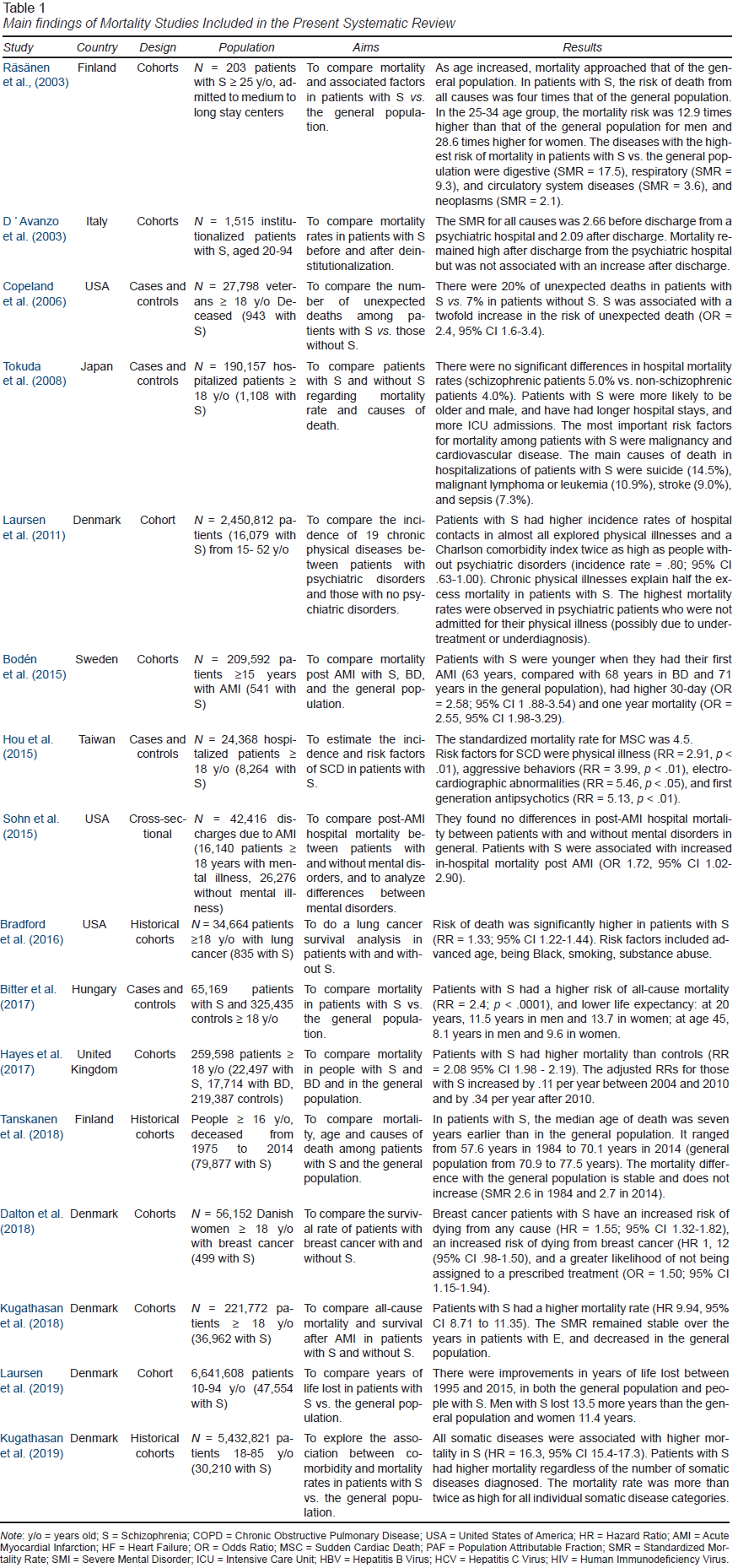
Mortality
The mortality rate of patients with schizophrenia is two to four times higher than that of the general population (Bitter et al., 2017; Bouza et al., 2010b; Gur et al., 2018; Hayes et al., 2017; Kugathasan et al., 2019; Laursen et al., 2019; Räsänen et al., 2003; Schoepf et al., 2014; Tanskanen et al., 2018; Table 1). In regard to sample size, the study with the largest sample was conducted by Tanskanen et al. (2018) in Finland, with 79,877 patients with schizophrenia, detecting a mortality rate 2.7 times higher than that of the general population. The study by Kugathasan et al. (2019) in Denmark was the second largest, with a sample of 30,210 patients with schizophrenia, obtaining a similar mortality rate, twice as high as that of the general population for all somatic diseases (from 2.16 per 1,000 in endocrine diseases to 2.85 per 1,000 in skin diseases).
The studies reviewed show that although patients with schizophrenia die from the same causes as those without this diagnosis, they have a shorter life expectancy. A Finnish study by Räsänen et al. (2003) of patients ages 25 to 34 found that the risk of mortality was 12.9 times higher for men and 28.6 times higher for women compared to that of the general population. Tanskanen et al. (2018) discovered that the gap in life expectancy was more significant among younger Finnish patients. Laursen et al. (2019) observed an increase in the number of years lost between 1995 and 2015 among individuals in Denmark. Specifically, men with schizophrenia lost 13.5 more years of life than the general population.
There appear to be disparities between authors in regard to the difference in life expectancy between patients with schizophrenia and the general population. In the United Kingdom (UK), Hayes et al. (2017) showed that hazard ratios (HR) adjusted for schizophrenia gradually increased from 2004 to 2009 and rapidly thereafter. However, Tanskanen et al. (2018) did not confirm this increase, as the standardized mortality rate for 79,877 Finnish patients with schizophrenia followed between 1975 to 2014 had remained stable for the previous 30 years.
Various studies have reported the diseases with the greatest impact on mortality. Kugathasan et al. (2019) found the leading causes of death to be respiratory, digestive, and cardiovascular diseases. Conversely, Bouza et al. (2010a) reported that circulatory, respiratory, and neoplasm cases accounted for 21%, 18%, and 17% of deaths respectively. In the article by Schoepf et al. (2014), the most common comorbidity in patients with schizophrenia was Type 2 Diabetes Mellitus (DM2). It was also a predictor of hospital mortality: alcoholic hepatopathy, Parkinson’s disease, Type 1 Diabetes Mellitus (DM1), kidney failure, ischemic stroke, pneumonia, ferrocene anemia, chronic obstructive pulmonary disease (COPD), and bronchitis.
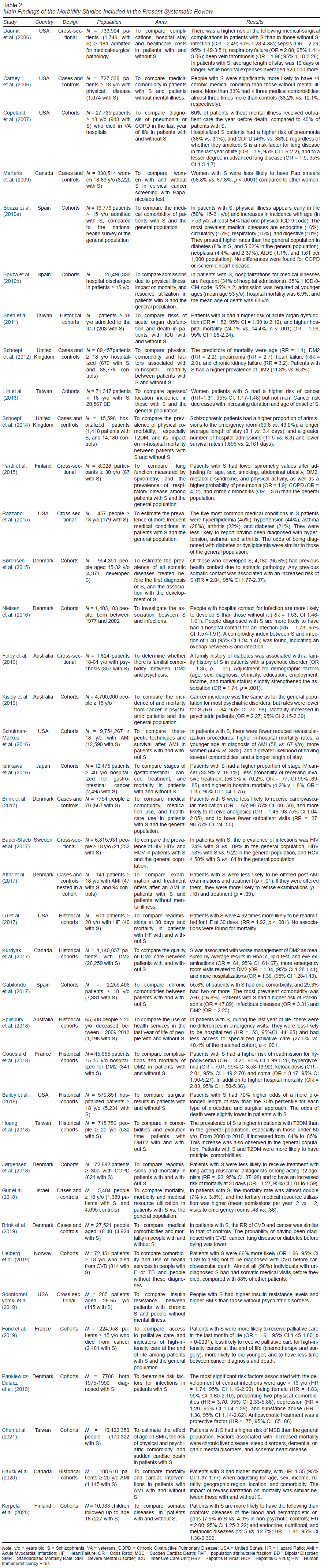
In terms of morbidity, the results reveal the following physical illnesses: cardiovascular diseases, respiratory diseases, Type 2 Diabetes Mellitus (DM2), oncologic diseases, and chronic infections (Table 2).
Cardiovascular diseases
Studies on mortality from post-hospital and long-term acute myocardial infarction (AMI) in North America and Northern Europe coincide with higher post-AMI mortality rates in patients with schizophrenia (Bodén et al., 2015; Hauck, et al., 2020; Kugathasan et al., 2018; Sohn et al., 2015). In Sweden, Bodén et al. (2015) compared 541 patients with schizophrenia with AMI with those with AMI without SMI. Patients with schizophrenia were younger at the time of AMI (with a mean age of 63) and had higher mortality rates (at 30 days). Kugathasan et al. (2018) studied 36,962 Danish patients with schizophrenia and AMI from 1980 to 2015 compared with the general population. They found higher mortality rates in patients with post-AMI schizophrenia at one and five years, and the absence of a decrease in the post-AMI standardized mortality rate.
In Taiwan, studies of sudden cardiac death (SCD) showed an increase in patients with schizophrenia (Chen et al., 2021; Hou et al., 2015). The largest study, led by Chen et al. (2021), of 170,322 patients with schizophrenia, found that 1,836 died of this cause. The standardized mortality rate was always > 1.00 and highest in male patients < 35 years of age. in addition, the risk scd increases with age, due to hypertension, and congestive heart failure, while drug-induced mental disorders decrease.
Respiratory diseases
Schizophrenia is associated with a higher probability of diagnosis of lung disease. The most extensive study was conducted at veterans’ hospitals in the United States by Copeland et al. (2007). In a sample of 28,000 patients, the 3.4% with schizophrenia had an increased likelihood of a diagnosis of lung disease during the last year of life, pneumonia and COPD, regardless of whether they smoked. The lack of outpatient medical care in the year before death was cited as an indicator of this increased risk.
Recent research conducted in Finland by Partti et al. (2015) suggested that individuals with schizophrenia may experience impaired lung function, as measured by spirometry. In Denmark, Jørgensen et al. (2018), found that patients with COPD and comorbid schizophrenia were less likely to receive long-acting muscarinic antagonists (MRI) or prolonged-acting ß2 agonists, putting them at a higher risk of mortality within 30 days. However, the study did not find any evidence of a higher risk of re-admission.
Type 2 Diabetes Mellitus
Studies agree that patients with schizophrenia have a higher prevalence of DM2. In the UK, Schoepf et al. (2012) indicated that the prevalence in patients with schizophrenia is 11.3%. In Denmark, exposure to antipsychotics was associated with ketoacidosis and DM2 in a previously non-diabetic population with schizophrenia (Polcwiartek et al., 2017). A family history of diabetes was associated with a family history of schizophrenia in an Australian study (Foley et al., 2016). In North America (Soontornniyomkij et al., 2019), patients with chronic schizophrenia had higher insulin resistance and higher body mass index (BMI). Moreover, an at-risk subpopulation was identified with a clinical profile (including negative symptoms, high BMI and being non-white) in which prevention of metabolic comorbidities was recommended. Conversely, in Canada (Kurdyak, et al., 2017), patients with diabetes and schizophrenia have lower rates of recommended tests and higher rates of diabetes-related hospital visits than patients with diabetes alone. Schizophrenia was associated with a reduced likelihood of optimal diabetes care, and an increased likelihood of emergency room visits and hospitalization.
Oncologic diseases
According to research conducted by Lin et al. (2013) in Taiwan, individuals with schizophrenia, particularly women, have a greater likelihood of developing various types of cancer. This study, which included 71,317 patients, suggested that the risk of cancer decreased with longer periods of schizophrenia and earlier diagnosis before the age of 50. The authors highlighted the incidence rates of colon, breast, cervix, and uterus cancers, which increased if schizophrenia was diagnosed after age 50. Nevertheless, Kisely et al., (2016) found lower cancer incidence rates in schizophrenia patients in Australia, although mortality increased across all psychiatric patients.
In another study with US veterans, Bradford et al. (2016) found factors associated with increased risk of death: being older, Black, smoking at the time of cancer diagnosis, and substance abuse. In regard to lung cancer, survival was significantly lower in patients with schizophrenia. Homeless shelter utilization was associated with a lower risk of death.
Concerning breast cancer, in Denmark, Dalton et al. (2018) found lower survival rates in patients with schizophrenia, since patients are less likely to be assigned to treatment.
As for cervical cancer, diagnostic procedures in Canada (Martens et al., 2009) have found that women with schizophrenia are less likely to have Pap smears to detect this type of cancer.
In regard to access to palliative care and high-intensity care at the end of life, a French national study (Fond et al., 2019) found that patients with schizophrenia were more likely to receive palliative care, less likely to receive curative care (chemotherapy and surgery), more likely to die younger, have a shorter lapse of time between cancer diagnosis and death, and more likely to develop chest cancers and comorbidities.
Chronic infections
Interestingly, in Denmark (Nielsen et al., 2016), it was found that people with hospital contact with an infection are more likely to develop schizophrenia than those without such an infection, and vice versa. Another Danish study (Pankiewicz-Dulacz et al., 2019) found that risk factors associated with severe infections in patients with schizophrenia are being young, female, having a medical comorbidity, and substance abuse. Moreover, a history of pre-diagnosis antipsychotic treatment was negatively associated with infections.
In Sweden, Bauer-Staeb et al. (2017) conducted a study to estimate the prevalence of blood-borne viruses (such as HIV, hepatitis B virus (HBV), and hepatitis C virus (HCV) in patients with SMI. Prevalence was higher in those with schizophrenia with HIV-.21%, HBV-.53%, and HCV-5.62%, with substance abuse contributing to this increased risk.
Information on the results of medical treatment and hospital access is provided in the following two sections.
Access to and Quality of Medical Treatment
Studies suggest that physical diseases in patients with schizophrenia are underdiagnosed and undertreated (Laursen et al., 2011). These patients are less likely to have required hospitalization in the year before death (Copeland et al., 2006). There were lower rates of diagnosis of cardiovascular disease, together with higher mortality rates (Brink et al., 2019; Correll et al., 2017; Heiberg et al., 2019) and utilization of tertiary medical resources. However, a study conducted in Israel by Gur et al. (2018) of 1,389 patients with schizophrenia, with follow-up for eight years, found that tertiary health care utilization was greater among patients with schizophrenia than among the general population.
A study conducted by Oud et al. (2010) in the Netherlands found that patients with psychotic disorders tended to have more frequent contact with their general practitioners (GPs), family doctors, including home visits, and telephone consultations. Additionally, they had a higher number of consultations overall. Patients aged 16 to 65 with psychosis and DM2, cardiovascular disease or COPD were assigned the same GP as other patients. Psychotic patients over the age of 65 had more frequent delirium. However, once these patients had been diagnosed, they were checked less frequently.
A study conducted in Australia (Spilsbury et al., 2018) showed there were more emergencies in a subgroup of patients with schizophrenia who died of cancer, asphyxiation, or intentional self-injury. Hospital admissions among those with schizophrenia were half those of patients without schizophrenia. However, these admissions increased by 50% when patients were treated in specialized palliative care, although patients with schizophrenia has less access to this type of care.
Hospital admissions
A study of medical-surgical discharges in the United States (Daumit et al., 2006) found that during their hospital stay, patients with schizophrenia have more complications than those admitted for the same reason without schizophrenia (such as more infections, respiratory insufficiency, deep vein thrombosis, and postoperative sepsis). These complications increase as these patients are at least twice as likely to be admitted to an intensive care unit (ICU) and to die (Daumit et al., 2006). Similarly, hospital mortality in the ICU was 10% higher in schizophrenic patients in Taiwan, with an increased risk of acute organic dysfunction (Shen et al., 2011).
Likewise, average length of stay is higher in patients with schizophrenia. An increase of at least ten days and a minimum of $20,000 in 2001 (Daumit et al., 2006) has been estimated, together with a 70% greater likelihood of remaining above the 75 percentile (Bailey et al., 2018). Indeed, a hospital in Greece (Douzenis et al., 2012) discovered that there is a direct correlation between the length of stay of a patient and the severity of their comorbidities, the latter being the most significant factor in prolonging their stay.
Discussion and conclusion
The main aim of this systematic review was to investigate the physical comorbidity of patients diagnosed with schizophrenia and the healthcare they received. The ultimate aim was to determine whether healthcare improvements in recent decades for the general population have positively impacted individuals diagnosed with schizophrenia.
The Impact of Physical Comorbidities on the Mortality of Patients with Schizophrenia
A crucial factor that could account for the increase in mortality in patients with schizophrenia is the extra medical care they receive compared to the general population (Moher et al., 2009). Patients with schizophrenia tend to receive palliative rather than curative treatment (Martens et al., 2009). Moreover, these patients are admitted for longer periods (placing them at a greater risk of infection) (Bauer-Staeb et al., 2017; Nielsen et al., 2016; Tokuda et al., 2008), yet have less access to early diagnosis (Brink et al., 2019; Heiberg et al., 2019; Laursen et al., 2014). We can therefore assume there is a lack of prevention and early intervention in these SMI patients globally that has persisted over time.
To improve the life expectancy of patients with schizophrenia, it is essential to create effective prevention plans to reduce the occurrence of physical illnesses in this vulnerable group, beginning with GPs. This task requires the involvement of both psychiatry and other medical specialties, with proper training, resources, and protocols in place, and strategies such as shared decision-making to ensure adherence to healthcare and medical protocols (Guadalajara et al., 2022).
Although the psychiatric care of patients with schizophrenia appears to have improved overall, as borne out by a 40% decrease in the number of suicides in this population (Tanskanen et al., 2018) between 1984 and 2014, the number of deaths due to physical causes such as cardiovascular disease and cancer has risen (Laursen et al., 2019; Nordentoft et al., 2021; Tanskanen et al., 2018).
Studies have shown that deinstitutionalization and liaison psychiatry have not significantly impacted mortality rates in patients with schizophrenia (D’Avanzo et al., 2003; Tokuda et al., 2008). To provide comprehensive care for these patients, it is essential to involve specialists from other areas of healthcare, particularly other physicians specializing in the comorbid illnesses detected.
Studies suggest that although the data are a matter for concern, individuals with schizophrenia are experiencing an improvement in longevity at a similar rate to the general population. However, a disparity remains as this population still has a life expectancy similar to that of the general population in 1988 (Laursen et al., 2019). One approach to reducing the metabolic impact of certain second-generation antipsychotics is to increase physical activity, which has shown promising results in various interventions (Gyllensten et al., 2020). Utilizing technology, such as mobile applications (mHealth apps), to improve lifestyle habits is an innovative, effective method worth exploring (Torous et al., 2017).
Physical Comorbidities with a Diagnosis of Schizophrenia
In regard to the principal physical comorbidities associated with this SMI diagnosis, our findings reveal a high prevalence of cardiovascular, respiratory and oncological diseases, significantly impacting the life expectancy of people with schizophrenia on every continent except Africa. The latest research indicates a rise in other illnesses (Laursen et al., 2014; Nordentoft et al., 2021).
Due to the characteristics of this psychiatric disorder, patients with schizophrenia are at a higher risk of contracting metabolic diseases, such as DM2, metabolic syndrome or cardiovascular diseases, which may be related to antipsychotic treatment, together with genetic and environmental factors (Bouza et al., 2010a; Foley et al., 2016; Korpela et al., 2020; Räsänen et al., 2003; Razzano et al., 2015; Tokuda et al., 2008). However indirectly, it has been found that these patients appear to use addictive substances associated with some of the physical comorbidities detected (such as cancer and SCD (Bradford et al., 2016; Chen et al., 2021; Kugathasan et al., 2019), the most harmful of which appears to be smoking nicotine or other substances.
A number of risk factors could therefore explain this increased risk: the tendency to lead a sedentary life (Vancampfort et al., 2017), treatment with atypical antipsychotics (Bernardo et al., 2021), the use of addictive substances (Bauer-Staeb et al., 2017; Kugathasan et al., 2019; Pankiewicz-Dulacz et al., 2019), difficulty understanding the disease itself (Oud et al., 2010), the absence of social support to access timely medical care, and the diagnosis, treatment or prevention of diseases (Laursen et al., 2011; 2014; Moher et al., 2009). Smart Screening could contribute to the early detection of physical comorbidities in patients and families if periodically provided in healthcare settings, as seen in initiatives in Mexico and Spain (Martínez-Nicolás et al., 2023a; 2023b).
The use of addictive substances (such as alcohol and tobacco), together with other unhealthy habits (such as a sedentary lifestyle and poor eating habits), could account for the increase in the incidence of these diseases (Correll, 2022). Tobacco use in patients with schizophrenia is estimated at between 49% and 80% (Hughes, 1993; Koskinen et al., 2009; Lasser et al., 2000). Conversely, alcohol abuse is estimated at around 20% (Contreras-Shannon et al., 2013), and a high BMI has been found in the profile of patients with schizophrenia and DM2. The development of atypical antipsychotics has enhanced the well-being of patients by reducing extra-pyramidal side effects. However, it has also led to an increase in metabolic-type side effects such as increased BMI and insulin resistance. Some antipsychotics have been found to elevate blood glucose levels and impair glucose tolerance, without involving intermediate mechanisms such as BMI (Stahl et al., 2009; Porras-Segovia et al., 2017). These effects could be attributed to the antagonism of MR cholinergic receptors, which could result in beta cell dysfunction (Poirier et al., 2002).
In addition, we discovered that patients with schizophrenia were receiving inadequate health care in comparison with the general population.
Healthcare utilization of Patients with Schizophrenia and Physical Comorbidities
The attitude of clinical professionals may be affected by the stigma of mental illness, such as patients’ inability to use appropriate healthcare pathways, which in turn prevents them from adequately addressing their health issues (Bitter et al., 2017). Social stigma (also present in physicians), healthcare availability (community-based psychosocial interventions), and economic policies are required to ensure that patients with SMI benefit from the scientific advances and lifestyle changes that have increased the longevity of the general population (Lee et al., 2018).
Other factors related to services and providers that may hinder the treatment of medical pathology include financial barriers, and lack of time, poor integration into services, or a shortage of proper screening measures. For instance, although psychiatrists are usually the main healthcare providers for patients with schizophrenia, they are not sufficiently trained to detect or treat physical diseases (Räsänen et al., 2003). Likewise, the detection of health issues related to lifestyle factors, while easily measurable, is often overlooked in healthcare screenings. Furthermore, reference tests for critical physical parameters are not administered with the required frequency, and individuals with SMI face an array of challenges, including modifiable lifestyle factors, in addition to other medical factors (such as the side effects of psychotropic medications, and inadequate access to quality healthcare (DE Hert et al., 2011).
Limitations
This study has certain limitations, including the absence of quality verification for the research selected and the heterogeneity of the articles reviewed, although the process has been led by psychiatrists. The methodological decisions regarding the selection of papers with specific methodological designs also limited the quantitative analysis of the data provided, which is why a meta-analysis was ruled out. It is therefore not feasible to perform a quantitative synthesis of the results and generalize them. Furthermore, there were no significant findings with regard to specific variables related to genetics, moderate or severe mental health issues, or even environmental factors. This highlights the need for further analysis of comorbidities that could be limiting the healthcare access and life expectancy of this population group.
Strengths
Nonetheless, the study has covered a broad spectrum, with the methodological rigor corresponding to the most recent discoveries. Despite these limitations, we were able to achieve our main aim of exploring key research on physical comorbidities in patients diagnosed with schizophrenia to determine their morbidity, mortality, and healthcare, in addition to presenting our findings in a clear, concise manner. Future studies could replicate the strategy by incorporating quantitative and meta-analytic approaches. They could also investigate psychosocial variables together with other specific variables to determine how healthcare actions could benefit this vulnerable population group and their families.
Conclusion
Patients with schizophrenia have a higher mortality rate than the general population due to cardiovascular, oncological, respiratory, diabetes, and infectious diseases, all of which are underdiagnosed and undertreated. Uneven medical care for these patients appears to be widespread across time and space. To minimize the effects of physical illness on this group of patients, it is essential to implement effective prevention and intervention strategies and programs. It is also important to provide training for clinicians across all levels of care, from primary to tertiary. Enhancing patient survival rates and improving their quality of life requires examining the correlation between psychosocial and socio-economic factors, substance addiction, antipsychotic drug use, healthcare access, and lifestyle choices in future research.